Partner Spotlight
“The Eyes at the Bedside”: How One Nursing@Simmons Grad Jumped into Action During COVID-19
Written by Stephen Eichinger on Jul 14, 2020
Related content: Graduate Programs, Digital Education

As an RN in a level 1 trauma ER, Taylor Campbell was used to dealing with life-or-death moments throughout her workday: gunshot wounds, automobile accidents, strokes, heart attacks. But not even her experience with these critical health scenarios could prepare her for what was to come: a major outbreak of a novel coronavirus.
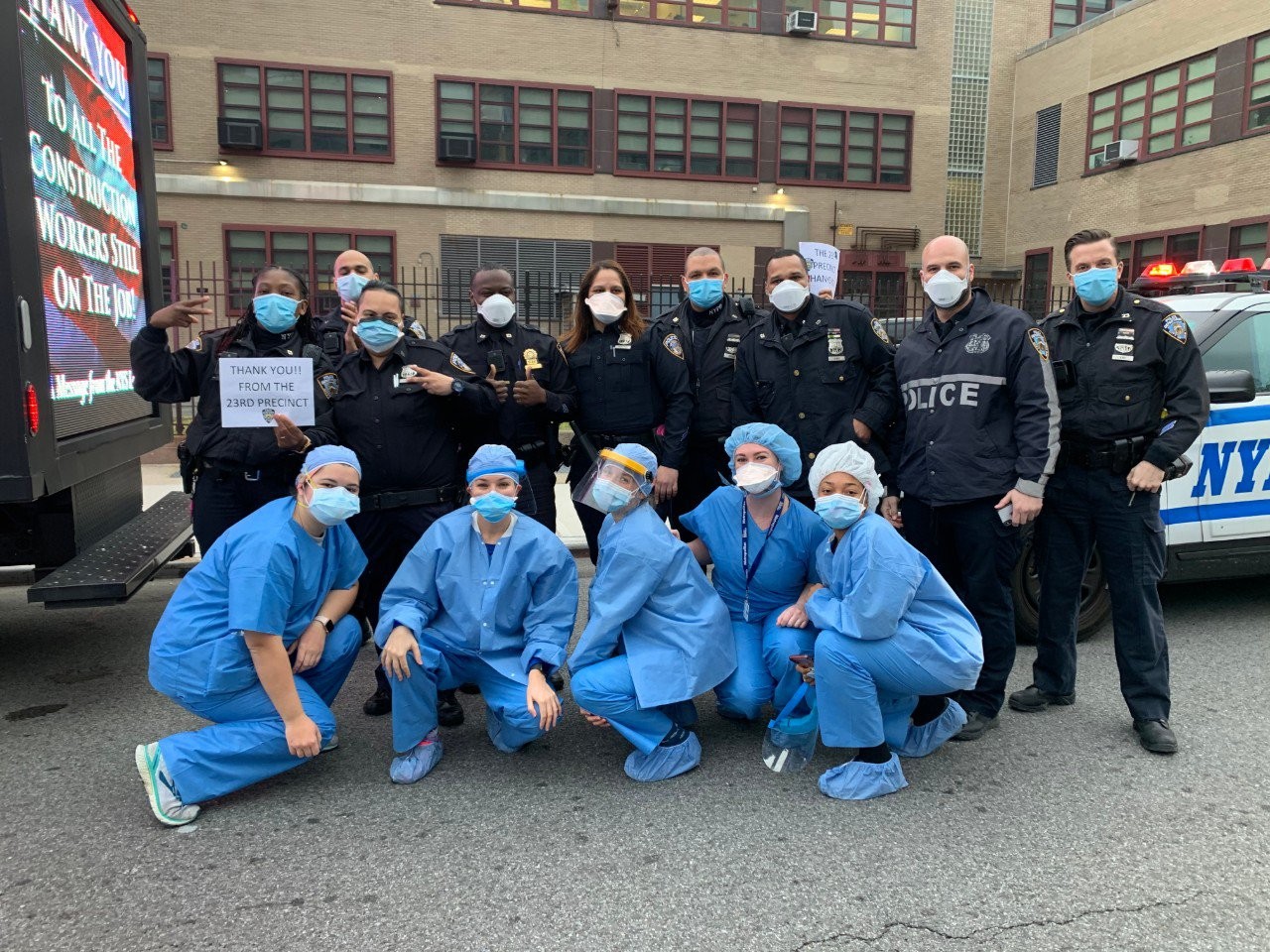
When COVID-19 began ravaging New York City, Taylor knew she wouldn’t be able to sit back in her home state of Rhode Island and do nothing. When the call came for health care volunteers to help out, she quickly packed a bag and headed down to the Big Apple.
Taylor had just graduated from the Simmons University online Master of Science in Nursing — Family Nurse Practitioner (FNP) program and had been studying to take her boards when the virus stalled her plans. Now she had another plan: help treat patients in the middle of a global pandemic. While voluntarily entering the US epicenter of a deadly virus comes with unquestionable risk, for Taylor it was part and parcel of her chosen profession.
“I just think that it’s our job as nurses,” she said. “We run toward danger.”
Advocating for her patients
For 21 straight days, Taylor worked at the Metropolitan Hospital Center in East Harlem. When she and her fellow volunteer health care workers initially arrived at the hospital, they discovered to their surprise that their first job would not be to treat patients but rather build the unit that would house them.
“They brought us to an abandoned floor of the hospital,” Taylor said. “No medical equipment, just beds. We had to stock it ourselves. It took us 48 hours to get it up and running.”
Once the patients did start coming, Taylor’s 12-hour shifts quickly became much longer due to the severity of the pandemic. “These are patients who are actively dying on you and you are trying to keep them alive,” she said.
The situation was made worse by the transmissibility of the virus. Taylor’s patients were not allowed guests because of the risk of spreading COVID-19. They were alone.
“In a normal situation, the patient would have family members at the bedside asking the doctor questions and talking about them,” Taylor said. “In this scenario, they don’t have family there. They’re intubated. They can’t speak. I’m the only person that is there for them.”
Even though the patients couldn’t verbally communicate with Taylor, she felt like she was able to get to know them. She described herself as “the eyes at the bedside.” The metaphor is apt for how Taylor views her work as a nurse.
“Being at the bedside in nursing is very important,” Taylor says. “Nurses know the patient. They know what the patient wants, and they are able to communicate with the doctors and ask the right questions. And often it gets the doctors thinking about different approaches to care or different solutions.”
Taylor describes nurses as patient advocates; it is a philosophy of care that the Nursing@Simmons program nurtures in its students.
“I'm one of those nurses that always wants to be learning and educating myself so that I can better advocate for my patients, and Simmons definitely helped me with that,” she says.
A Nursing@Simmons clinical placement crystallizes Taylor’s commitment
While in the Nursing@Simmons program, one of Taylor’s clinical placements was in the pediatric unit of the Providence Community Health Centers, a nonprofit health care facility and the only Federally Qualified Health Center (FQHC) in Providence, Rhode Island, that provides quality primary health care services to a diverse population. Working with children was a big shift for Taylor, who had only ever experienced adult-serving ERs. But she enrolled in the Nursing@Simmons program to be able to take care of people across the lifespan, so she was eager to get the experience. With any of her patients, she believes as strongly in helping prevent illness as she does in prescribing medicine when illness does strike.
“I like being able to educate and explain how to do that primary prevention, which Simmons does a very good job of focusing on,” Taylor said. “Preventing people from getting sick, educating about high blood pressure and diabetes, helping people change their diet—introducing these measures early. I think that is very important, and part of the reason I chose Simmons.”
Taylor says her clinical placements with underserved populations helped her as she began her COVID volunteer work in New York City. “Simmons stresses culture and diversity so that definitely helped going into the city,” where the virus was impacting communities of color at a disproportionate rate.
Moving forward as an FNP
Following Taylor’s service in New York, she returned home for a quick break before she resumed the plans she had pre-COVID: studying for the boards. She recently learned that she passed, so she is now a board certified family nurse practitioner.
While Taylor is looking forward to the next chapter in her nursing career, she can’t help but reflect on the thoroughly exhausting yet undeniably heroic time she spent in New York City—in particular how she felt every morning before the bus picked her and her colleagues up for yet another shift facing down a virus that was the cause of so much illness and death.
“Even if you had the worst day the day before, you were there for a reason,” she said. “We had a purpose. And off we went.”
Latest.
Learn more about us.
At 2U, we’re on a mission—to eliminate the back row in higher education and help universities thrive in the digital age. To learn more about who we are and what we do, follow the links below.