Partner Spotlight
Caring for the Whole: Meet Two Nursing@Georgetown Preceptors Who Are Key to Student Success
Written by Jessica Wang on Sep 21, 2021
Related content: Graduate Programs, Leadership, Strategic Partnerships
Cura personalis. Georgetown University’s tradition in health care of “caring for the whole person”—an individual’s total physical, emotional, social, and spiritual health—resonates through every aspect of the School of Nursing & Health Studies’ (NHS) online Nursing@Georgetown programs. This tradition applies not only to how Nursing@Georgetown students are educated to care for their patients, but also to how preceptors work with students in their clinical placements all around the country.
As the experienced practitioners who supervise students at clinical placement sites and facilitate their application of theory into practice, preceptors are an indispensable part of student learning in Nursing@Georgetown, which celebrates its 10th anniversary this year. To date, over 1,600 students have graduated from the online program with a 98% board passage rate. In total, they’ve also clocked over one million clinical hours at placement sites across the country, and they’ve delivered over 10,000 babies. So in my role as 2U’s senior vice president of placement, I witness inspiring examples of preceptors’ impact every day.
The preceptors, whom we help NHS identify, select, and secure, possess a strong passion for teaching, learning, service, and a desire to both “give back” and propel their profession forward. Their unwavering commitment to students truly enables 2U to double down on our mission: They help us not only eliminate the back row in education but also eliminate gaps in American health care—particularly for women, people of color, LGBT individuals, families in poverty, and others in need.
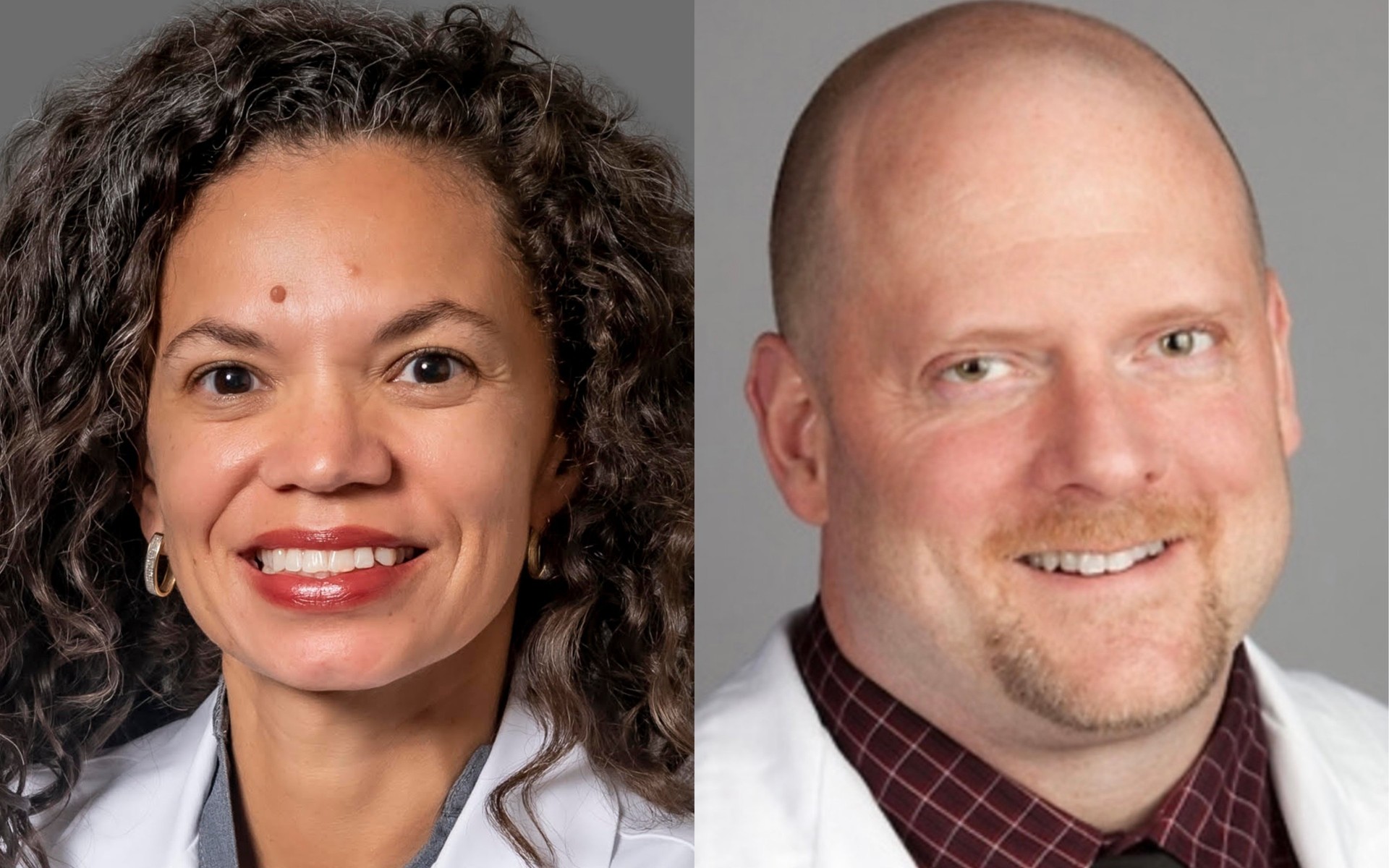
To showcase the influential role that preceptors play, we connected with two preceptors who have each mentored several Nursing@Georgetown students over the years: Jessica Brumley, a Certified Nurse Midwife (CNM) and the director of the Division of Midwifery for University of South Florida (USF) at Tampa General Hospital, and Gary Foster, a Family Nurse Practitioner (FNP) and the director of clinical operations at Agape Clinic in Dallas, Texas, who is also an Air Force veteran and a 2015 graduate of Nursing@Georgetown. Read on to learn why they became preceptors, how their practice adds value to the learning experience, and how their appreciation for Nursing@Georgetown students speaks to the program’s commitment to quality.
What compelled you to become a preceptor?
Jessica Brumley (JB): I serve on the board of the American College of Nurse-Midwives. We constantly talk about how the country needs more midwives, but the biggest barrier is a lack of clinical placement sites dedicated to midwifery education. I want to make sure midwives have quality hands-on learning experiences and that they’re inspired to become preceptors down the road. As a preceptor at USF, I get to work with everyone at the hospital, which helps remove this sense of “us vs. them,” nurses and midwives vs. physicians. Preceptors are the bridge; we’re the role models showing everyone how to build collegial relationships, speak the language of respect and teamwork but also autonomy, and help support more team-based care in the future.
Gary Foster (GF). Throughout my entire nursing career, I was essentially doing the work of a preceptor—teaching, mentoring, and advising—so it was a natural choice. Becoming clinic director allowed me the opportunity to formally take on the role of a preceptor and bring on more Georgetown students so that they can benefit from what we see at Agape. There’s a need for nurses to experience the patient population we work with here, mostly undocumented immigrants and the working poor. Because we’re a free clinic, 100% paid by private and corporate donations, we’re a very unique placement option. That’s why I was drawn here in the first place.
We have these wonderful collaborative physician partnerships that help everyone learn from each other. Plus, we get a good sense of students’ strengths and weaknesses to be able to play to their gifts and work on areas needing more attention.— Jessica Brumley, CNM and director of the Division of Midwifery, University of Southern Florida
How does your clinical placement experience add value for students?
JB: USF serves all kinds of patients, so it’s a great opportunity for students to get a lot of in-depth midwifery training. Ethnically and economically, the range is extremely diverse. We serve low-risk patients having a normal, healthy birth but also high-risk patients who need every intervention under the sun. Since we’re an academic medical center, it’s a very interprofessional practice. We educate students to be midwives, OB-GYNs, doctors, and PAs, so we have these wonderful collaborative physician partnerships that help everyone learn from each other. Since two or three of us work with the same student, there’s more scheduling flexibility and continuity over time. Plus, we get a good sense of their strengths and weaknesses to be able to play to their gifts and work on areas needing more attention.
GF: Agape gives students experience working with a wide range of patients, particularly indigent populations, both in terms of minority and financial status. It’s a well-rounded placement that aligns with Georgetown’s mission of helping those less fortunate. I give them as much hands-on autonomy as possible, which lets them practice to the fullest extent they’re allowed, but with me as a safety net. They get to develop a patient’s history, do their physical exam, come up with a working diagnosis, maybe even conduct a procedure they wouldn’t have been able to work on elsewhere. They present it to me and I verify everything they’ve proposed, make any adjustments, and then we proceed with treatment.
Clinical placements can have a powerful impact on the community. How is that the case with your practice?
JB: Florida has one of the highest c-section rates in the nation. I’m proud we send so many midwives around the state to practice in their communities, ready to tackle this challenge. We also partner with several community-based midwives in the region, and I think the birth community is appreciative of our collaborative relationship. My team serves as a bridge between the hospital and these home and birth center midwives, because sometimes their patients need more intensive care. These relationships help make the transfer of care easier in those situations and help patients feel better about being handed from one midwife to another.
GF: As a free clinic, the way Agape operates is similar to a military facility. Most of these folks have nowhere else to go for medical care, so if they come in asking for help, we give it to them. And if we don’t already have what they need, we find a way to get it. Before COVID, we were seeing 4,000-6,000 patients a year. Since the pandemic, it’s been 18,000 patients a year. Ninety-eight percent of our patients speak Spanish. Our students benefit from being on the front lines of all of this. And the patients in our community also benefit from this special teaching and learning environment.
I truly enjoy working with Nursing@Georgetown students. Not just because I also came from that program, but because I’ve never hosted a single one who hasn’t been prepared. They excel in their ability to jump right in and put themselves to the test.— Gary Foster, FNP and director of clinical operations, Dallas’ Agape Clinic
Have you had any memorable Nursing@Georgetown student experiences that reflect the program’s commitment to quality?
JB: Early on as we were growing our group, one of the first midwives I hired was a Nursing@Georgetown graduate. She was about to drive two-and-a-half hours each day to another part of the state for her next rotation, and she had a new baby at home that she was still breastfeeding. She was incredibly dedicated to midwifery. But we asked, do you really want to be doing that? We brought her on board, and she was fantastic. From then on, she set the bar really high for future hires.
GF: Of all the students I get, I truly enjoy working with Nursing@Georgetown students. Not just because I also came from that program, but because I’ve never hosted a single one who hasn’t been prepared. Some students from other programs may not see the potential for all they can get out of the placement. I’ve always said that you don’t learn anything by “holding up the wall” and standing around and observing. You don’t understand what all is involved until you’re put on the spot. Nursing@Georgetown students excel in their ability to jump right in and put themselves to the test.
What are the greatest rewards that come from precepting?
JB: I love seeing my former students out in the community. Many of them are now my colleagues and they’re reaching out to me for advice. It’s helping me continue to build my network, for sure. But really, it’s all about the joy of watching a student at the end of their placement, who’s nearly independent and self-sufficient, blossoming into the kind of provider we want to see in the world.
GF: Working with students forces me to stay current and sharp. And of course, I have a vested interest in Nursing@Georgetown’s success as one of its graduates. I’m just honored to be able to have an impact on students who will one day be in my shoes, and on the patients and families I serve. As nurse practitioners, the patient is at the center of everything we do. Not medicine, not treatment, but the human being at the center of it all. It’s a very fulfilling perspective.
````
Interested in learning what it’s like to be a student in the Nursing@Georgetown programs? Read this interview with two different generations of alumni who had a unique clinical placement experience.
Latest.
Learn more about us.
At 2U, we’re on a mission—to eliminate the back row in higher education and help universities thrive in the digital age. To learn more about who we are and what we do, follow the links below.